As individuals age, their health needs also change. One area that deserves special attention is gut health, especially when taking medications. Gut health refers to the state of your gastrointestinal (GI) system. This includes:
- Digestion
- A normal and stable microbiome
- Absence of gastrointestinal illness and disease
- An effective immune system
Gut health is linked to many other aspects of your health. This means emotional stress and chronic illnesses affect and are affected by the GI system. Specific foods, behaviors, and environments affect an individual’s gut health.
Taking medication can disrupt the delicate balance of gut bacteria, particularly antibiotics. Proton pump inhibitors, NSAIDs, and more also affect them. By understanding these effects, seniors can make informed choices and take control of their health. This article explores the following subtopics:
- Gut microbiome
- Common medications that impact it
- Strategies to maintain gut health during treatment
The Gut Microbiome: A Crucial Ecosystem
The microbiome refers to all the bacteria, viruses, and fungi in your body. The bacteria are on your skin, mouth, throat, colon, and everywhere in your body. There are 10,000 different microbial species in the human body. They are categorized as aerobic and anaerobic. The former needs oxygen, while the latter doesn’t. These microbiomes influence different health conditions, from cancer to COVID-19.
The gut microbiome contains over 100 trillion microbes. They influence digestion, nutrient absorption, and immunity. This complex ecosystem aids the following processes:
- The breakdown of carbohydrates
- The production of vitamins
- The protection against infection
Age-related changes in gut bacteria impact the absorption of nutrients and medications. Finding a primary care doctor with the right expertise can help alleviate stress for seniors. This can seem daunting, but their skills and experience will assist seniors in creating a diet and lifestyle that’s beneficial to their gut health.
How Medications Disrupt Gut Balance
Many commonly prescribed medications profoundly disrupt the gut microbiome’s delicate balance. They potentially contribute to adverse health effects in both the short and long term.
Antibiotics: Double-Edged Swords
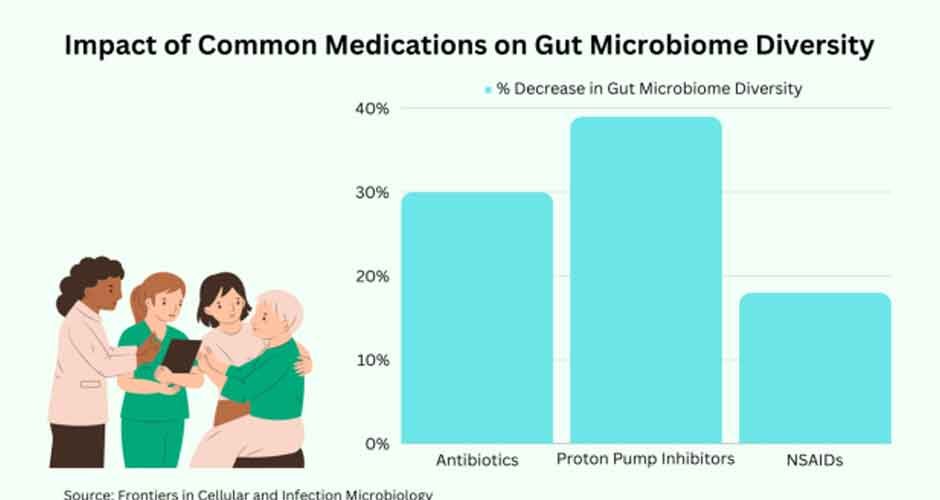
Antibiotics are invaluable for fighting infections caused by harmful bacteria. However, they also indiscriminately kill off beneficial gut bacteria. Just one 7-day course of antibiotics can decrease the diversity of gut bacteria by 30%. The effects can last up to a full year. This drastic imbalance in microbial communities is linked to the following:
- Antibiotic-associated diarrhea
- Intestinal infections like C. difficile
- Impaired nutrient absorption
- Reduced immunity
Some antibiotics disrupt gut flora more extensively than others. Broad-spectrum antibiotics target a wide range of bacteria. They typically have more impact compared to narrow-spectrum versions. Tetracycline causes a 10x greater drop in gut microbial diversity compared to penicillin. For the elderly, the consequences of antibiotics on gut health should always be weighed heavily. It’s especially important when considering treatment options.
PPIs: Balancing Acidity and Consequences
Proton pump inhibitors (PPIs) such as omeprazole powerfully reduce stomach acid production. They are routinely prescribed for heartburn, ulcers, and acid reflux. However, long-term PPI use significantly alters the gut microbiota. It increases the risk of developing an intestinal Clostridium difficile infection by 74%.
Suppressing stomach acid also impairs the absorption of key nutrients. This includes vitamin B12, calcium, iron, and magnesium. This effect is particularly worrying for the elderly. They are already at risk for nutritional deficiencies. There is also emerging evidence linking long-term PPI use with higher rates of dementia.
NSAIDs: Balancing Pain Relief and Gut Health
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are heavily used by seniors. It is to relieve arthritis pain and inflammation. However, NSAIDs are directly toxic to the lining of the stomach and intestines. Remarkably, up to 65% of regular NSAID users end up experiencing the following conditions:
- Increased intestinal permeability
- Ulcers
- Bleeding
- Worsening of underlying conditions like Crohn’s and colitis
The gastrointestinal effects of NSAIDs can be severe for older adults. This is especially true when layered on top of the decline in gut barrier function. This highlights the importance of reducing NSAID intake and taking preventative steps to protect the gut.
Strategies for Maintaining Gut Health
Certain strategies can aid in counteracting the medication-related gut issues experienced by many seniors:
Probiotics and Prebiotics
Probiotic supplements containing strains have been shown to assist in rebalancing gut flora. They restore healthy function both during and after antibiotic treatment. Examples of those include like Lactobacillus and Bifidobacterium. Support gut bacteria with prebiotic fibers from foods like onions, garlic, and bananas. They provide further benefits.
Timing of Medication
Taking antibiotics and NSAIDs with food aids to protect the stomach lining from irritation. Maintaining consistent timing of medication in relation to meals is also key. Abruptly changing this routine can impact proper absorption. Always follow instructions from healthcare providers about timing.
Communication with Providers
Discussing medication side effects and concerns with doctors allows for the customization of treatment plans. It can be tailored to an individual’s needs. Over 30% of seniors experience adverse drug reactions from prescription medications. This highlights the vital importance of clear communication with healthcare providers. In effect, this will improve treatment and gut health.
Finding a primary care doctor you trust and can communicate openly with is a great first step. Bringing up gut-related symptoms early provides more opportunity for adjusting medications. It will also give the elderly a chance to change lifestyle approaches. Seniors should feel empowered to speak up and make informed choices. This is especially true about drug treatments that impact their gut microbiome.
Frequently Asked Questions
Can probiotics interfere with medications?
Probiotic supplements are generally considered safe to take alongside medications. However, it is best to consume them a few hours apart from any prescription drugs and always verify with your doctor.
How can I reduce antibiotic side effects?
Take antibiotics with food to reduce stomach irritation. When possible, opt for narrow-spectrum versions targeting specific bacteria. Boost gut health during and after treatment with fermented foods, or probiotic supplements. Yogurt and kefir are among the most popular choices.
What dietary changes support gut health during medication use?
Focus on getting more prebiotic fibers from sources like garlic, onions, leeks, asparagus, and bananas. Stay well hydrated with water, bone broths, and herbal teas. Consider anti-inflammatory herbs like ginger to soothe the GI tract. Avoid gut irritants like coffee, alcohol, and spicy foods.
The Bottom Line
Medications like antibiotics and NSAIDs impact the gut microbiome. Strategies like probiotics, prebiotics, and open provider communication can counteract these effects. Paying attention to gut health is key for seniors to enhance their nutritional status and medication absorption during necessary treatments.



